Promoting Healthy Skin Microbiome
"Our hope is that by correcting bacteria on the skin, [eczema] patients won’t have to do constant treatment."
"Those bacteria [colonizing the skin of eczema patients] are deficient compared to the same bacteria taken from a healthy volunteer."
"We have done some genetic testing that tells us definitively that those bacteria are different. We took the bacteria from healthy people and we saw that the bacteria does everything you would want it to do to improve atopic dermatitis in a petri dish and in mice. In mice, we can actually make their disease go away with this bacteria."
Dr. Ian Myles, National Institute of Allergy and Infectious Diseases, National Institutes of Health

That certainly compares most favourably with, for example, a new eczema drug which the Food and Drug Administration has recently approved called Dupixent, an injectable drug that comes with a $37,000 yearly price tag to help ease the intolerable itch, swelling, redness and crusting (typical of the most sever cases of eczema) that comes with eczema. And while most such medications come in the form of creams or lotions whose purpose is to soothe eczema inflammation (atopic dermatitis), this new drug alters the immune system response underlying inflammation, as a monoclonal antibody.
That's the old way of treatment, and Dr. Myles and his colleagues feel that they are on to something simpler and possibly far more 'natural', and useful in its capacity to overturn the disharmony of skin microbiota whose faulty presence promotes the presence of eczema. Dr. Myles and his researchers appear to have validated in their research that the species of bacteria populating the skin of people with eczema while appearing the same as those of healthy people, are in reality weak and incapable of guarding against harmful bacteria like Staphylococcus aureus.
Theirs is not the only research team attempting to prove that good bacteria can help treat eczema.
The National Institutes of Health is also funding research whereby Dr. Richard Gallo of the University of California, San Diego and his colleagues are working on producing a lotion with two benign staph bacteria -- Staphylococcus hominis and Staphylococcus epidermidis -- to challenge the harmful effects of the Staphylococcus aureus.Dermatologist and biologist Dr. Gallo has concocted with his colleagues what is considered an innovative microbial eczema treatment.
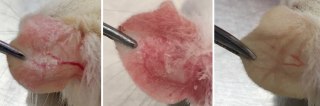
The discovery that Dr. Gallo made was that Staphylococcus hominis and Staphococcus epidermis have the capacity as friendly microbiome, to kill Staphylococcus aureus, known to be involved in eczema production. S. hominis and S. epidermidis were swabbed from volunteers' skin with eczema to grow the bacteria in the laboratory, then to produce a lotion incorporating the microbes. Following which the balm was applied experimentally to the forearms of volunteers, vastly increasing their own helpful skin bacteria.
The results were seen in 24 hours when the probiotic lotion succeeded in almost eliminating S.aureus from the volunteers' skin. Enabling the researchers to identify compounds used by the beneficial bacteria to deter S.aureus. Their results were published in Science Translational Medicine. Last year another study had Dr. Gallo and other researchers inject a beneficial strain of Staphylococcus epidermidis with food it digested into mice ears, thus encouraging the growth of S.epidermidis, in turn reducing both the number of P.acnes and the level of inflammation.
A team in South Korea and the United States demonstrated that an extraction from Heliocobacter pylori, commonly found in the human stomach, also can inhibit P.acnes, decreasing skin inflammation in mice, in 2014. It was demonstrated by scientists in Canada that people who take both probiotics and antibiotics result in significantly fewer acne lesions in the space of 12 weeks, in comparison with others taking only one or the other.
These promising new treatments' potential have alerted private companies to the obvious, that they want to be next in line to capitalize on a growing market for consumers prepared to switch their preferences to probiotic cosmetics, toiletries and topical treatments, even to the point where one enterprising biotech company now promotes a "live probiotic spray", to replenish beneficial skin bacteria.
As far as Dr. Gallo is concerned, his experimental lotion represents an "evolutionarily honed" treatment. "There are so many new potent medicines right under our nose", he stated.
Labels: Bacteria, Biochemistry, Health, Medicine

0 Comments:
Post a Comment
<< Home