Laser Surgery: What could Go Wrong With Minimally Invasive Techniques?
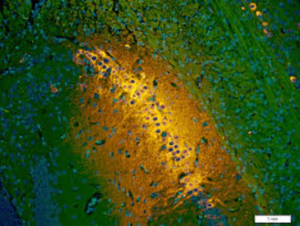
"In the course of cervical dilation in preparation for the hysteroscopy, the left fundal myometrium was perforated. The perforation was suspected by the surgeon based on the sudden absence of resistance on the dilator during cervical dilation. The perforation was subsequently confirmed with hysteroscopy. The perforation did not extend the time required to complete the surgery or prevent completion of the operative hysteroscopic portion of the surgery, which included resection of intrauterine adhesions and endometrial polypectomies. With release of the fluid pressure during the hysteroscopy, there was minimal bleeding from the perforation site, and there was no blood emanating from the cervix following the procedure. No interventions were required to treat the complication. Uterine perforation during cervical dilation is a known complication of this procedure that is of infrequent occurrence. In this case, the presence of intrauterine adhesions may have contributed to this event."
"The patient had a hysteroscopy done [at the beginning of the week] in the surgical center. The patient returned to the emergency room [the following day] and was sent to the OR that evening. Investigation showed she had a perforated uterus and small bowel perforation from the [hysteroscopy] to remove fibroids."
Commonwealth of Pennsylvania
"It's a two-dimensional [keyhole incisions in minimally-invasive surgery] look at what's in three dimensions."
"We're training surgeons differently; there's much more simulation [in laparoscopic surgery]."
"Young surgeons have much more real, laparoscopic experience."
"The important point is that although safe, things do sometimes not go well. And we're trying to alert the profession as to what the issues are so they can further reduce any preventable harm." Dr. Gordon Wallace, managing director, Canadian Patient Safety Institute

In laparoscopic surgery there is a public understanding that because it is minimally invasive in nature, unlike 'open' surgery where large openings are made in a patient's body to permit more complicated surgical procedures, the less intrusive method translates to smaller scars, less bleeding, less pain, and swifter post-surgical recovery. All of which, generally speaking, is certainly true. Without taking into account complications like accidental perforations which are admittedly few in number.
But with "keyhole" incisions, their very size of entry and sightlines creates another type of complication where it becomes challenging for surgeons to visualize, rather than view the anatomy to see the placement of viscera and to protect internal organs during the small-incision surgical proceedings. Half of the most serious complications ensuing from small incisions, according to studies, relate to the insertion of a surgical tool called a trocar.
Insertion of the trocar is performed "blindly"; in essence with the surgeon judging where it should go and then proceeding with the hopeful assurance that all will go well. Sometimes it does not. The surgeon, after all, cannot actually see where the trocar he has inserted is going; if it becomes inserted too deeply, too swiftly with too much pressure, or off-angle, complications can and will raise their ugly heads.
A 24-year-old man, for example, died during emergency appendix surgery at a Calgary hospital in 2010 when a surgeon blindly inserted into the patient's abdomen a sharp-bladed trocar, slicing a major artery and the patient could not be resuscitated. But according to Dr. Wallace of the Canadian Medical Protective Association, such accidents, rare as they are, are being minimized even further as surgeons gain more experience.
A review of such mishaps revealed instances of doctors who fail to respond to a "deteriorating" situation by changing tactics to immediately alter the surgery to an open type, giving the operating physician more control of the situation. Because complications develop and the surgeon is unable to see into the body what may be happening, the swift response required does not occur because the surgeon may be oblivious to the situation unfolding, since some injuries fail to be detected until the post-op period.
"Even then, surgeons sometimes failed to consider the possibility of a surgical injury", observed the Canadian Medical Protective Association's review of 423 closed cases where laparoscopic surgery was found to have occasioned injuries related to lacerated or damaged bowels, blood vessels, reproductive organs or nerves, as well as delays in recognizing and treating those injuries. The issue of surgeries performed on the wrong body part, or on the wrong patient also came under scrutiny.
Of the 423 cases reviewed, covering cases between 2011 and 2015, 45 people died of the complications that ensued from their minimally-invasive surgeries. Experts reviewing these cases found reason to be critical of care provided to patients in 74 percent of the surgeries under review.
Hysterectomy and other gynecological procedures, cholecystectomy (gallbladder removal), appendectomy and nephrectomy (kidney removal) were the most frequently involved laparoscopic procedures.
In one perhaps typical case, a surgeon made an incision into a patient's navel, then inserted a sharp-bladed trocar to produce a portal into the abdominal cavity where instruments and cameras can be passed during surgery. The surgeon, finding resistance in inserting the trocar, pushed a little harder, accidentally puncturing the woman's abdominal aorta. The injury went undetected, and the blood pooled, causing significant nerve damage, leaving the woman with chronic, debilitating pain.
Many other injuries related to the puncturing or laceration of bile ducts during gallbladder surgery. Bile spilled into the abdominal cavity can cause potentially life-threatening infections. An inquiry resulting from a death placed the blame on improper use of a bladed trocar that was disposable, instead of a blunt, reusable trocar. Though the surgeon was highly skilled he had "experienced a momentary lapse in judgement that caused him to believe that he could use the bladed trocar safely", according to the judge.
"In open surgery, everything is done under direct visualization, so there’s much, much less chance of an inadvertent injury from a puncture or something. [However], there are certain techniques we call open techniques where you don’t use a sharp trocar though the skin. You make a small opening in the skin, you directly expose so you can see inside the abdominal cavity without putting anything in in a blind way."
"A lot of surgeons would consider these techniques in general to be safer than blind insertion techniques, where a sharp instrument is placed inside the abdominal cavity without clearly seeing the entire trajectory of the instrument."
"It’s not like these are totally new, that surgeons wouldn’t have any clue that it’s an issue and that you have to watch out for it. Surgeons who do minimally invasive surgery are by and large aware of these techniques for doing these types of manoeuvres, and getting access to surgical sites."
Dr. David Urbach, surgeon-in-chief, Women’s College Hospital, Toronto

Labels: Bioscience, Health, Surgery